Osteoarthritis
What is Degenerative Osteoarthritis: Understanding the Degenerative Joint Disease
Introduction:
Osteoarthritis is a prevalent degenerative joint disease that affects millions of people worldwide. With its impact on joint health, it is important to understand the causes, symptoms, diagnosis, and available treatment options for this condition. In addition, as a board-certified Regenerative Orthopedics & Sports Medicine doctor at the Institute of Regenerative Orthopedics & Sports Medicine (IROSM) in Fort Lauderdale, Florida, I am dedicated to providing comprehensive care to individuals dealing with osteoarthritis.
Defining Osteoarthritis:
Osteoarthritis is a chronic condition characterized by the degeneration and breakdown of joint cartilage. furthermore, it commonly affects weight-bearing joints such as the knees, hips, and spine. This degenerative process leads to pain, stiffness, and limited mobility in the affected joints. Also, osteoarthritis is the most prevalent form of arthritis and can significantly impact an individual’s quality of life.
Understanding Joint Health:
Joints play a crucial role in our body’s movement and flexibility. They connect bones, provide support, and allow for smooth articulation. In the other hand, healthy joints are essential for overall well-being, enabling us to engage in various activities and maintain an active lifestyle. Proper joint function relies on the integrity of joint structures, including cartilage, synovial fluid, and surrounding ligaments and muscles.
Causes and Risk Factors:
Several factors contribute to the development of osteoarthritis. Age is a significant risk factor, as joint degeneration becomes more common with advancing age. Genetic predisposition can also play a role, as certain individuals may be more susceptible to cartilage breakdown. Joint injuries, obesity, and repetitive stress on joints due to certain occupations or sports activities can increase the risk of osteoarthritis.
Signs and Symptoms:
Osteoarthritis manifests through various signs and symptoms. Joint pain, especially during movement or after prolonged periods of inactivity, is a common complaint. Stiffness in the affected joints, reduced range of motion, and swelling may also be present. These symptoms can significantly impact daily activities, such as walking, climbing stairs, or gripping objects.
Diagnosis:
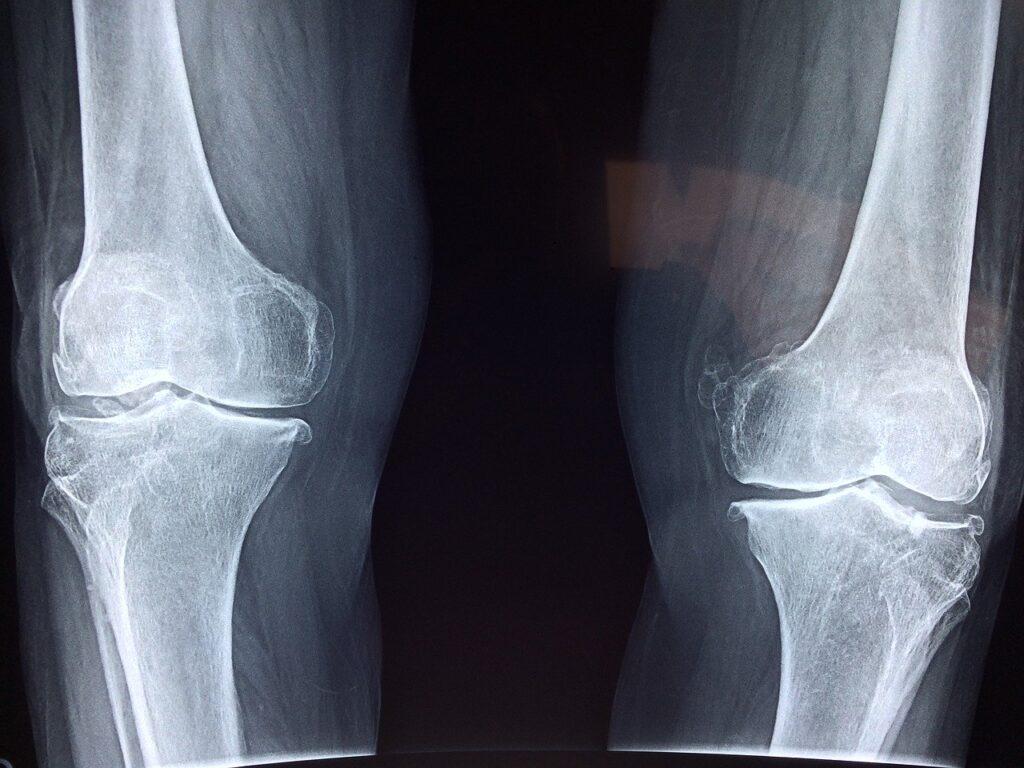
To diagnose osteoarthritis, a comprehensive evaluation is necessary. This typically involves a thorough medical history review, physical examination, and imaging tests. Furthermore, medical professionals will assess the location and severity of joint pain, examine joint movement, and may request X-rays, MRI scans, or CT scans to visualize joint structures and evaluate the extent of cartilage damage.
Differentiating Osteoarthritis from Other Conditions:
While osteoarthritis shares similarities with other forms of arthritis, it has distinct characteristics that differentiate it from conditions like rheumatoid arthritis, gout, psoriatic arthritis, and septic arthritis. Unlike inflammatory arthritis, osteoarthritis is primarily a degenerative process, affecting specific joints rather than the entire body. The diagnostic criteria and underlying mechanisms also differ.
Classification and Stages of Osteoarthritis:
Osteoarthritis can be classified into primary and secondary types. Primary osteoarthritis is associated with the natural aging process and wear-and-tear on joints. Secondary osteoarthritis, on the other hand, occurs as a result of specific conditions, such as joint injuries, obesity, or congenital joint abnormalities. The severity of osteoarthritis can be classified into different stages, ranging from mild to moderate and severe, based on the extent of cartilage damage and joint dysfunction.
Osteoarthritis in Specific Joints:
Osteoarthritis can affect various joints in the body, with the knees, hips, hands and fingers, and the spine being commonly affected. Each joint presents unique challenges and requires specific treatment approaches. For instance, knee osteoarthritis may benefit from physical therapy, weight management, and, in some cases, surgical interventions like knee replacement. Understanding the impact of osteoarthritis on specific joints helps tailor treatment plans to individual needs.
Risk Factors and Prevention:
While some risk factors for osteoarthritis, such as age and genetics, are beyond our control, there are measures we can take to reduce the risk and slow the progression of the disease. Maintaining a healthy weight, engaging in regular exercise, protecting joints from injuries, and practicing proper joint biomechanics can help prevent or delay the onset of osteoarthritis.
Treatment Options:
The treatment of osteoarthritis involves a comprehensive approach aimed at relieving pain, improving joint function, and enhancing quality of life. Non-surgical treatment options include medication for pain management, physical therapy to strengthen muscles around the affected joints, the use of assistive devices for mobility support, lifestyle modifications such as diet and exercise, and complementary therapies like acupuncture or herbal supplements.
Surgical Treatment:
In cases of advanced osteoarthritis where conservative measures are ineffective, surgical interventions may be considered. Joint replacement surgeries, such as hip or knee replacements, can provide significant pain relief and improve joint function. Arthroscopy, a minimally invasive procedure, may be performed to repair or remove damaged cartilage. Osteotomy, a surgical realignment of bones, can also be an option for select cases.
Regenerative Orthopedics and Sports Medicine:
Regenerative orthopedics offers innovative approaches to osteoarthritis treatment. Techniques such as platelet-rich plasma (PRP) therapy, stem cell injections, and growth factor treatments aim to stimulate the body’s natural healing processes and promote tissue regeneration. As a board-certified Regenerative Orthopedics & Sports Medicine doctor, I specialize in these advanced treatment modalities to help patients find relief from osteoarthritis symptoms.
Coping Strategies and Emotional Support:
Dealing with osteoarthritis can be emotionally challenging, as chronic pain and physical limitations can impact mental well-being. It is essential to address the emotional aspect of the condition and develop coping strategies. Seeking support from family, friends, and support groups can provide valuable emotional support. Additionally, healthcare professionals can offer guidance on pain management techniques and psychological interventions.
Advancements in Osteoarthritis Research:
Ongoing research and advancements in the field of osteoarthritis hold promise for future treatment options. Regenerative medicine, including tissue engineering and gene therapy, shows potential for cartilage repair and regeneration. Emerging technologies and interventions aim to improve early detection, personalized treatment plans, and long-term outcomes for individuals with osteoarthritis.
Conclusion:
In conclusion, understanding what is degenerative osteoarthritis is crucial for individuals experiencing joint pain, stiffness, and limited mobility. By recognizing the signs, seeking professional medical advice, and exploring appropriate treatment options, individuals can effectively manage the impact of osteoarthritis on their lives. As a board-certified Regenerative Orthopedics & Sports Medicine doctor at the Institute of Regenerative Orthopedics & Sports Medicine (IROSM), I am dedicated to providing comprehensive care and improving the quality of life for those dealing with osteoarthritis. Remember, early intervention and a multidisciplinary approach are key to managing this degenerative joint disease successfully